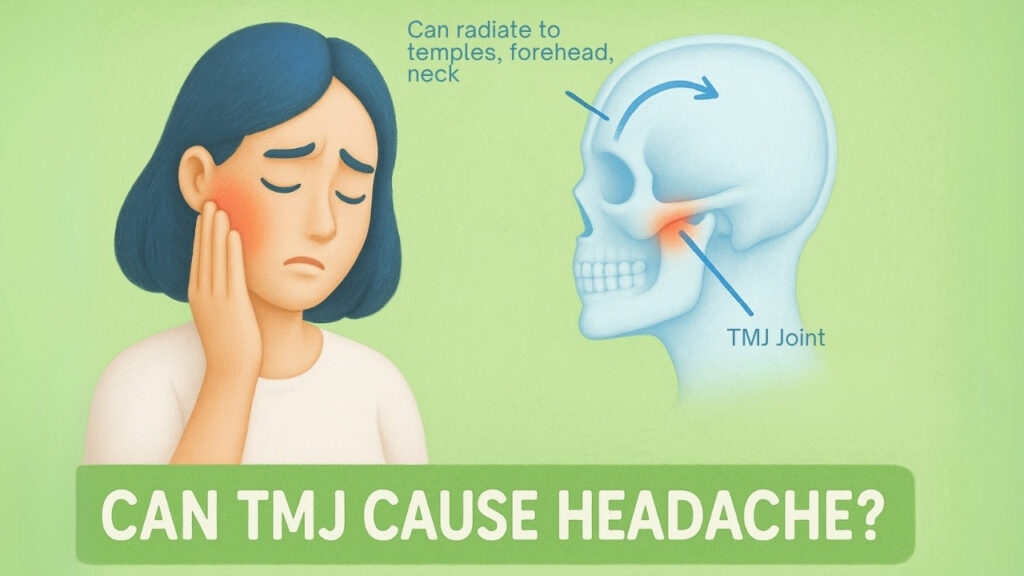
If you’ve ever had jaw tension turn into a throbbing headache, you’re not alone, and the culprit could be your temporomandibular joint (TMJ). This joint, located near your ears where your jaw connects to your skull, is responsible for everyday actions like chewing, talking, or yawning. But when something goes wrong with it, the effects can ripple far beyond your jaw. One of the most commonly reported, yet often misunderstood. Symptoms of TMJ disorders are chronic headaches.
So, is there a real connection? Can issues with the jaw joint actually cause headaches that feel like migraines or tension-type pain? Let’s break it down in a clear, evidence-backed, and balanced way.
What Is TMJ and Why It Matters for Headaches?
The TMJ isn’t just any joint, it’s a complex, sliding hinge joint that allows your jaw to open and close, glide side to side, and perform those chewing motions we rarely think about. On each side of your head, right in front of your ears, this joint works in tandem with muscles, ligaments, and a disc of cartilage that keeps everything smooth and cushioned. When the joint, surrounding muscles, or the disc get irritated or misaligned, that’s when we run into trouble, what’s broadly called a temporomandibular disorder (TMD).
TMDs represent a group of over 30 conditions affecting the joint, jaw muscles, and associated nerves. Importantly, the term “TMJ” refers to the joint, while “TMD” refers to the disorders affecting it. These disorders are the second most common cause of chronic pain, affecting between 5% and 12% of the population. Interestingly, only a small portion require surgery, meaning most cases are manageable with conservative care.
Studies, like those from the American Migraine Foundation, suggest TMDs can show up in a variety of ways: jaw pain, chewing difficulty, joint locking, facial pain, clicking noises, earaches, and yes, headaches. In fact, headaches are one of the most commonly reported symptoms of TMDs, affecting up to 79% of patients. These headaches are frequently misdiagnosed as migraines or tension headaches because the pain can radiate to the temples, behind the eyes, or even the neck and shoulders.
| Mechanism | Description | Key Associated Factors |
|---|---|---|
| Muscle Tension | Dysfunction in the TMJ leads to tension, knots, or spasms in jaw and surrounding muscles (e.g., temporalis, masseter), radiating pain to the head. | Bruxism (teeth clenching/grinding), Muscle overuse, Trauma, Psychological stress, Myofascial trigger points |
| Nerve Compression | Misalignment or inflammation within the TMJ can compress or irritate nearby nerves, particularly branches of the trigeminal nerve, triggering pain signals. | Trigeminal nerve involvement, Nerve sensitization (peripheral and central), Inflammation, Jaw misalignment |
| Vascular Changes | Inflammation and swelling in the TMJ area can affect local blood vessels, disrupting normal blood flow and contributing to headache development. | Inflammation, Swelling, Altered blood flow dynamics |
| Referred Pain | Pain originating from the TMJ or associated structures is perceived in other areas of the head, face, or neck due to shared neural pathways. | Myofascial trigger points, Temporal Tendonitis, Ernest Syndrome, Complex neural pathways |
Common Symptoms of TMJ Disorders
Temporomandibular disorders present with a broad spectrum of symptoms, with headache being a highly prevalent manifestation, reported by 79% of affected individuals. Beyond headaches, a constellation of other symptoms frequently accompanies TMDs:
- Pain or tenderness in the jaw and/or temporomandibular joint: This is often cited as the most common symptom after headache, affecting the chewing muscles and/or the joint itself.
- Aching facial pain: Discomfort can spread across the face.
- Pain spreading to the face, shoulder, neck, or back: Pain can radiate significantly beyond the jaw area.
- Difficulty chewing or pain while chewing: Essential jaw functions become compromised.
- Clicking, popping, or grating sounds in the jaw: These noises occur when opening or closing the mouth. It is important to note that such sounds, in the absence of pain or limitation of movement, are common and typically do not require treatment.
- Limited jaw movement or locking of the joint: This can make it difficult or impossible to fully open or close the mouth.
- Earaches or ringing in the ears (tinnitus): These symptoms are not caused by an infection of the inner ear canal but are referred from the TMJ region.
- Neck pain: Often co-occurs due to the interconnected musculature.
- Eye pain: Can be a referred symptom.
- Tooth pain or sensitivity: May occur in conjunction with jaw tenderness.
- Dizziness: Another potential referred symptom.
- Changes in bite alignment: Alterations in how the upper and lower teeth fit together can be indicative of TMJ issues.
- Bruxism (teeth clenching or grinding): Reported by 58% of TMD patients.
Why TMJ and Headaches Are Often Connected?
Several physiological mechanisms help explain why TMJ dysfunction can lead to headaches:
- Muscle Tension & Myofascial Pain: TMD often involves spasms or tightness in muscles like the masseter and temporalis. These can create myofascial trigger points, tiny knots that refer to pain across the head and neck. Over time, this muscle tension creates a cycle of pain and inflammation that triggers chronic headaches.
- Trigeminal Nerve Irritation: The TMJ sits near the trigeminal nerve, which is responsible for much of the facial and cranial sensation. When the TMJ is inflamed or misaligned, it can irritate this nerve, leading to pain that radiates into the head. The trigeminal nerve also connects with pain pathways in the brain, creating overlap between jaw issues and head pain.
- Central Sensitization: Chronic TMJ dysfunction can alter how the brain processes pain, making even minor stimuli feel more intense. This concept explains why some people with TMD become increasingly sensitive to stress, sound, or light, hallmarks of migraine.
- Vascular Changes: Inflammation around the joint may also interfere with blood flow in nearby vessels, contributing to headache patterns similar to migraines.
- Referred Pain: Some TMD-related pain originates from nearby ligaments and tendons. Conditions like Temporal Tendonitis and Ernest Syndrome can mimic classic headache pain, further blurring the lines.
Who Gets TMD the Most?
TMD is most common in adults between ages 20 and 40, and it affects women more often than men. Some reasons people develop TMD include:
- Grinding or clenching teeth (called bruxism)
- Stress and anxiety
- Accidents or injuries to the jaw
- Poor posture
- Problems with how the teeth fit together
So, Can TMJ Really Cause Headaches?
Yes, it can. And not just one kind:
- Tension headaches from tight muscles
- Migraine-like pain from irritated nerves
- Neck-related headaches when jaw and neck problems overlap
Research shows that treating TMJ problems can help reduce how often or how badly people get headaches. But it’s important not to assume one always causes the other. That’s why doctors look at all your symptoms together, like jaw pain, clicking, or earaches, before making a diagnosis.
What’s the Best Way to Treat TMJ-Related Headaches?
If you’re having headaches that seem to start from your jaw, you might be dealing with TMJ issues. The good news? There are lots of ways to feel better, most of them simple and safe. You don’t have to rush into surgery. Doctors say it’s best to start with easy, non-permanent options and only move to bigger treatments if needed.
Let’s walk through your choices in a simple and helpful way.
Start with Easy Fixes at Home
Many people find relief with conservative, at-home changes. These methods are safe, affordable, and often effective for managing both jaw pain and headaches:
- Soft food diet: Eating softer foods reduces the load on the jaw. Avoid tough, sticky, or chewy items.
- Heat and cold therapy: Apply moist heat to relax the muscles or cold packs to reduce swelling. Use for 15-20 minutes several times a day depending on pain type (heat for chronic tension, cold for acute flare-ups).
- Jaw rest posture: Keep your tongue on the roof of your mouth, teeth slightly apart, and lips closed. Avoid excessive jaw movement or wide yawning.
- Reduce bad habits: Avoid chewing gum, nail-biting, and leaning your chin on your hand.
- Improve posture: Slouching can tighten neck and jaw muscles. Good sitting posture eases that strain.
- Stress management: Use techniques like meditation, deep breathing, journaling, or yoga. Stress is a major factor in jaw clenching and headaches.
Physical Therapy and Jaw Exercises
Gentle movement and Physical Chiropractic therapy from our Dr. Eumi can help relieve tension, improve mobility, and prevent recurring pain. Exercises may include:
- Chin tucks and side glides: To strengthen and align jaw muscles.
- Goldfish exercises: Simple open-close motions while maintaining correct tongue position.
- Massage and stretching: Reduces stiffness and breaks up trigger points.
- TENS therapy, moist heat, ultrasound, or laser therapy: May be used under therapist supervision.
These methods can reduce the severity and frequency of TMJ-related headaches by addressing muscle-based pain patterns and referred tension.
Mouthguards and Splints (Oral Appliance Therapy)
Custom nightguards can:
- Reduce teeth grinding (bruxism)
- Minimize jaw pressure while sleeping
- Help realign the bite slightly to reduce strain
Note: These should not permanently change your bite. Avoid over-the-counter hard plastic guards unless guided by a dentist, as they can worsen symptoms if misused.
Try Medicine Carefully
Medications can be helpful when used cautiously and as part of a broader care plan:
- NSAIDs (ibuprofen, naproxen): For inflammation and short-term headache or jaw pain relief
- Muscle relaxants: Useful for acute muscle spasms but not long-term solutions
- Tricyclic antidepressants (e.g., amitriptyline): Helpful in chronic pain cases, especially when sleep is disrupted
- Propranolol: Can be effective when TMJ pain overlaps with migraines
Avoid opioids, they’re not recommended due to high addiction risk and low effectiveness for TMJ.
Mind-Body Approaches and Behavioral Therapies
Pain isn’t just physical, it’s emotional and behavioral too. These tools can change how you process and respond to pain:
- Cognitive Behavioral Therapy (CBT): Helps manage chronic pain and stress responses
- Biofeedback: Teaches muscle relaxation using sensor-guided feedback
- Self-education and mindfulness: Empower you to take control of your condition and reduce fear around pain
These are especially helpful if stress or anxiety worsen your jaw tension or headaches.
Other Treatments You Might Hear About
Sometimes people ask about more aggressive options. Here’s what research and experts say:
- Botox injections: This was suggested by the Health Pain Institute that it may reduce muscle pain in severe cases, but it’s not FDA-approved for TMJ and may not help with joint issues. Results are temporary (3-4 months), and long-term safety is still being studied.
- Dry needling or trigger point injections: May help break up muscle knots in the jaw. More evidence is needed, but some report short-term relief.
Low-level laser therapy or acupuncture:Studies show mixed results. May help some people but is not a guaranteed solution.
Be Careful with Surgery or Big Changes
Experts are very clear: permanent treatments should only be used in rare, well-diagnosed cases. This includes:
- Arthrocentesis or arthroscopy: Used to remove debris or reposition a disc. Minimally invasive but not always long-lasting.
- Open-joint surgery: High risk, limited evidence of long-term success, and may worsen symptoms. Only considered for severe, structural damage.
- TMJ implants: Artificial joints come with serious risks. Historically, many implants failed. Long-term studies for newer versions are still needed.
- Bite-changing dental work: Like grinding teeth down or orthodontic realignment, these should be avoided unless absolutely necessary. They can make symptoms worse.
Always get second opinions, and never agree to a permanent treatment without understanding the risks.
Combining Treatments for Best Results
The best approach is usually a mix:
- Self-care and stress reduction
- Physical therapy or exercises
- Conservative medical help when needed
PMC Case studies show that people often improve with splint therapy and lifestyle changes. For example, a 24-year-old with severe TMJ pain and headaches improved by 80% after using a splint and medication like naproxen over two months.